Mental illness and social exclusion: An evaluation of a recovery-oriented rehabilitation programme
Caterina Balenzano
Department of Political Sciences, Università degli studi di Bari Aldo Moro, Italy
Giuseppe Moro
Department of Political Sciences, Università degli studi di Bari Aldo Moro, Italy
CORRESPONDENCE:
Caterina Balenzano
e-mail: caterina.balenzano@uniba.it
Abstract
Relational approaches in contemporary health-care and social work practice were used by many helping professions who adopt a strength-based approach aimed at promoting users’ recovery. From a relational practice perspective, many recovery-oriented programmes have been experimented within mental health services’ field.
Using mixed methods, the paper investigated the coherence, effectiveness and social impact of a recovery-oriented programme (MeNS) implemented in a southern Italian mental health service. First, the study analysed how recovery markers were adopted by MeNS staff using interviews and focus group discussions. Second, a two-group evaluation design compared 50 MeNS beneficiaries and 100 patients treated by traditional rehabilitation paths in terms of recovery, using both Recovery Style Questionnaire and a Recovery Assessment Scale. Finally, the beneficiaries’ quality of life and the programme’s social impact were explored with data from a focus group with beneficiaries and journal articles on MeNS and social stigma. The results highlighted that MeNS is a recovery-oriented programme capable of confronting patient stigmatisation and promoting their recovery and quality of life by a relational social work paradigm. The implications for health policies and practices were discussed, underlining the need to design services effective in promoting user quality of life and social inclusion.
Keywords
Relational approach, recovery, mental illness, psychiatric rehabilitation, programmes’ evaluation.
Introduction
Recovery represents one of the most used paradigms in health and social services’ management and health and social policies’ planning (Clementi, 2019). According to the recovery approach, people who have been stigmatized for their problems can be appreciated by society by redefining their life challenges (Davidson, 2012). As one of the pillars of the Relational Paradigm of Social Work (RPSW, Folgheraiter, 2011), mental health service users, family members, and citizen experts work together with practitioners with technical expertise.
RPSW emphasizes the individual’s capacities to achieve change also by their social networks and considers people in need of support as persons with capacities and capabilities within their social networks with which they can achieve the required change. Because RPSW focuses on relationships as the basis for change among all the people involved in coping process, practitioners identify and resolve problems by facilitating coping networks to improve both individual and collective resilience and capacities (Folgheraiter & Raineri, 2017). So, RPSW asks people to adopt a strength-based approach towards helping each other, thus representing a real challenge to social work practice.
Avoiding stigmatisation and encouraging a change in terms of social inclusion of people with severe mental illness (SMI), including by improving their employment opportunities and relational networks, is a central goal of territorial mental health services (MHSs) adopting a recovery-oriented approach (ROA). Recently, considerable progress in this direction has been made in psychiatric rehabilitation practices. ROAs have been recognised as best suited for psychiatric rehabilitation in severe mental disorders (Xu et al., 2018), and new intervention models have been developed to help patients with SMI improve the skills necessary to live positively within the community (Roessler, 2006) and recover a role in their family, social groups and society (Liberman, 2008).
Recovery and the community-based approach to mental health rehabilitation
In recent years, treatment of SMI has shifted from a «simple» pharmacological action to manage symptoms to «new» activities aimed at promoting patients’ functional recovery (Vita & Barlati, 2019) and social inclusion by creating a Therapeutic Rehabilitative Project (TRP) integrated as far as possible within the social context (e.g. Vita et al., 2016). Following the European recommendation to combating Stigma and Social Exclusion of persons with SMI (European Commission, 2010), policy makers and stakeholders have tried to combine self-help and self-management activities to encourage personal recovery with initiatives based on a community-based approach aimed at decreasing inequalities, stigma and discrimination, and at promoting social inclusion of those with SMI.
On the one hand, MHSs following a community-based approach are increasingly offering patients activities in the community as a key aspect of the rehabilitation process. In accordance with the social contact theory, professionals promote direct contacts and interactions between those with SMI and the community, considering this to be an effective strategy both in overcoming social distance and reducing mental health stigma and for promoting patients’ social inclusion, thereby breaking the cycle of discrimination on mental health grounds. This approach has contributed to better patient quality of life, greater satisfaction with the services used (Tansella & Thornicroft, 2009), and a change of attitude and behaviour towards them (Couture & Penn, 2003).
On the other hand, recovery-oriented services and practices, widespread in many countries across the world (Allott et al., 2009), recommend the integration of standard medical approaches with psychosocial rehabilitation programmes (including, for example, family psychoeducation, illness self-management training and social skills training), in order to encourage patient functional recovery (Layard, 2006; Kern et al., 2009).
However, there is continuing uncertainty about what «recovery» means in the context of mental illness (Bonney & Stickley, 2008). In literature, despite repeated attempts to formulate a universally acceptable «working definition» of recovery, this construct has been described in many ways: as a guiding principle; as a set of outcomes; or as a set of processes (Corrigan & Ralph, 2005).
When conceptualised as outcome, recovery refers to overcoming symptoms and returning to standard functioning (the patient’s state); when defined as a process, it is measured as the termination of despair, having meaningful goals, the revival of hope, a purpose in life and more positive experiences, regardless of the presence of recurring symptoms (Rudnick, 2012; Shamir, 2012). According to Anthony’s key definition (1993, p.15), recovery involves the development of new meaning and purpose in one’s life as one grows beyond the catastrophic effects of mental illness. In all these cases, however, scholars have emphasised patient personal development, self-esteem and quality of life, within the constraints of their mental illness (e.g., Anthony, 1993; Leete, 1989; Unzicker, 1989), conceiving «wellness» and «illness» as independent variables. By changing their attitudes, values, feelings, goals, skills and roles, people with SMI develop personal comfort (Ralph, 2000) and a new meaning and purpose in life (Davidson, 2012; Roe et al., 2007); thus, they can live a satisfying, hopeful and meaningful life as citizens of their communities, beyond the limitations resulting from their psychiatric symptoms (Anthony, 1993; Deegan, 1993).
Despite both the awareness of promoting a ROA in mental health systems (Shepherd et al., 2010) and practices (Roberts & Hollins, 2007) and scholars’ efforts to define what recovery-oriented services look like, it remains unclear how the recovery principles should be defined in mental health policy and practice (Farkas, 2007). There is, therefore, a need to explore more thoroughly both how treatment can facilitate the recovery process of those with SMI, and how the relationship between professionals and mental health consumers might facilitate recovery and promote social inclusion.
Furthermore, current recovery-oriented rehabilitation practices are very variable across countries, both in methodology and content. Specifically, in Italy, several approaches and techniques co-exist: some are targeted at promoting patients’ independent living; others try to facilitate patients’ understanding of their mental health disorder (psychoeducational interventions); others focus on personal and environmental care. The most common first-line interventions are pharmacological, while TRP is often considered «second line», and psychosocial treatments are rarely implemented for at-risk mental states. Moreover, when different, individual independent experts carry out rehabilitative interventions, their differing professional beliefs represent a significant barrier in designing a homogenous, recovery-oriented TRP aimed at meeting patient needs through interdisciplinary treatment. Finally, in Italian «real-world» rehabilitative settings, patients with SMI are often not involved in the development of TRP and rarely participate in service evaluation, organisation or management (Vita et al., 2016).
For all these reasons, the development and implementation of recovery-oriented services and practices within services in Italy need to be better described and evaluated.
Background and evaluated programme
The MeNS programme represents an innovative experience born in southern Italy (in the city of Bari) from the need to convert a day-centre for patients with SMI into a new «healthcare network», where professionals from not-for-profit organisations and specialists belonging to public MHSs collaborate, from the assessment of patient needs to the design of a rehabilitation programme. This rehabilitation strategy aims to reduce residential long-term care and the associated health costs, as well as improving patients’ social inclusion in the community and promoting their wellbeing through recovery-oriented interventions carried out by a multidisciplinary team. It sets out to strengthen patients’ positive strategies, reinforce competences weakened by mental disorder, and stimulate autonomy. The specific planned actions which form part of TRP take place in different everyday life contexts and promote patients’ social, relational and communicational skills through social interactions with those without SMI. This operating model is practised as a first-line programme and is experienced with the active participation of patients, who thereby contribute to their own self-determination, even if they have at-risk mental states.
Research questions and design
This study is aimed at answering the following research questions.
- Is the MeNS programme a recovery-oriented programme? Has the programme the key features of the ROA? How have the markers of the recovery approach been contextualised in the MeNS programme? (Evaluation of coherence).
- Are the different pathways to care and rehabilitation (recovery-oriented vs. traditional) associated with different levels of patients’ perceived recovery? (Evaluation of effectiveness).
- Is the recovery-oriented pathway to care linked to lower stigmatisation and a better quality of life? (Evaluation of effectiveness and social impact).
For the first question, the evaluation of coherence analysed how the markers of the recovery approach were adopted by the MeNS programme; this was done by exploring the views of coordinators and professionals, through an interview and focus group discussion (FGD) respectively.
For the second question, a two-groups comparison evaluation design was used. At the beginning of the research (t0), psychiatrists clinically observed patients and indicated their diagnosis, in accordance with the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013). Using a three-point scale, clinicians also assessed patients’ (a) degree of malfunctioning (mild, moderate, severe); (b) motivation to change; (c) compliance with treatment; (d) therapeutic alliance; (e) cooperation of family (poor, sufficient, very good). After the assessment, patients were assigned to the two models of the programme. Patients involved in A group participated in integrated programmes combining pharmacological and psychotherapeutic interventions with recovery-oriented activities and personalised activities promoted in the social community to reduce stigmatisation: psychoeducation; illness self-management training; different creative laboratories; and group social skills training. Patients in B group benefited only from traditional psychosocial rehabilitation involving pharmacological and psychotherapeutic interventions. After the two rehabilitation programmes were compared (t1), participants completed a self-report survey aimed at measuring their recovery.
For the third question, the quality of life and stigmatisation of patients involved in the MeNS programme were examined by combing data derived from one FGD involving patients, and information selected from some articles in newspapers relating to this experience. Firstly, patients were asked to reflect on their pathway in the MeNS programme, describing their stigmatisation and quality of life before and after the MeNS; secondly, publications and journal articles about the MeNS programme were selected for analysis to highlight the social impact of the programme in terms of social stigma.
The study design was approved by the Local University Research Ethics Committee. The respondents were not paid for their participation. They completed an informed consent and were advised that any information provided was confidential and they could withdraw at any time from the study.
Method
Participants
The FGD with professionals involved all 10 professionals belonging both to public and to private organisations who make up the MeNS staff: one psychologist, one psychiatrist, four health educators, two psychiatric rehabilitation therapists, and two social and health personnel. The FGD with beneficiaries involved 5 patients (two women and three men in adulthood) willing to share their personal history of illness and rehabilitation.
The sample of the quantitative study includes a total of 150 individuals with SMI receiving treatment in MHSs. In order to be included in study sample, patients had to meet the following inclusion criteria: having a diagnosis of mental illness; being aged 18 or older; living in the community; and being capable of filling out the study survey independently. Among the selected cases, 50 were involved in the MeNS programme (A group), and 100 in traditional psychosocial rehabilitation (B group). Among patients of this last group, 50 were treated in the same MHS where the MeNS programme was experienced (B1 group), while the other 50 were treated in another MHS (B2 group). In this way, we were able to take into account both the influence of the treatment and the role of the context in which the PTR was made. All the participants were born and live in Italy. 47.3% of patients were male; 52.7% female. The mean age was 45.76 years (SD= 12.56). Table 1 summarises the diagnostic clusters of mental disorders according to the DSM-V classification system.
|
Diagnostic clusters |
% |
|
Neurodevelopmental disorders |
2.7% |
|
Schizophrenia spectrum and other psychotic disorders |
27.7% |
|
Bipolar and related disorders |
16.2% |
|
Depressive disorders |
25% |
|
Anxiety disorders |
6.1% |
|
Obsessive-compulsive and related disorders |
5.4% |
|
Neurocognitive disorders |
2% |
|
Personality disorders |
14.9% |
|
Total |
100% |
Table 1 Clinical data
Instruments and measures
Both the interview with the MeNS coordinator and the FGD involving professionals were focused on analysing MeNS aims (question 1), distinctiveness (question 2) and types of recovery-oriented methods and practices (question 3). The FGD with patients was focused on the most significant practices and activities during the TRP (question 1), and the main changes in their relationships with/in their community and in their lifestyle, thanks to this experience (question 2).
The interview with the MeNS coordinator lasted about one hour; the staff FGD lasted about two and half hours; the patients’ FGD lasted about one and half hours. The same researcher interviewed the coordinator and facilitated the discussion among all the participants during both the FGDs, while a research assistant audio-recorded and later transcribed the contents of each of the three events. Seven newspaper articles about the MeNS programme were selected for analysis.
The quantitative self-report survey had two parts: the first part collected socio-demographic information; the second part included the following self-reporting scales administered to measure recovery as a process.
The Recovery Assessment Scale (Corrigan et al., 1999) represents one of the best measures of personal recovery (Cavelti et al., 2012) as a process (Corrigan et al., 2004); it is useful in evaluating studies examining the recovery-orientation of MHSs or programmes. It is a 41-item scale, linked to a five-point agreement scale (5 = strongly agree; 1 = strongly disagree), organised in the following five factors/subscales: (1) personal confidence and hope; (2) willingness to ask for help; (3) goal and success orientation (e.g., «I have a desire to succeed»); (4) reliance on others; and (5) not being dominated by symptoms (e.g., «I can handle it if I get sick again»). The first factor corresponds with the constructs of confidence and self-determination; factors 2 and 4 with the ability to reach out to others; factor 3 appears to correspond to the empowerment associated with recovery; factor 5 with patients’ coping strategies. The RAS total score, obtained from the answers to all 41 items, has been found to be positively associated with empowerment and quality of life and inversely associated with psychiatric symptoms. Research investigating the psychometric properties of the RAS original version has shown that the scale has satisfactory reliability and validity scores (Corrigan et al., 1999; McLoughlin and Fitzpatrick, 2008; O’Connell et al., 2005; Salyers et al., 2007), good internal consistency measured by Cronbach’s alpha (McLoughlin & Fitzpatrick, 2008; O’Connell et al., 2005; Salyers et al., 2007), and an adequate stability over a two-week period (Salyers et al., 2007). The RSA has also demonstrated a good content validity, assessed from consumer and other stakeholder perspectives (O’Connell et al., 2005) and satisfactory convergent and discriminant validity (Salyers et al., 2007). The Italian version also showed good psychometric properties, both in the first Italian adaptation study (Boggian et al., 2011) and in the more recent validation study (Boggian et al., 2020): the internal consistency of the RAS total score showed excellent (α = .93), while the convergent validity is good. In line with the results from Corrigan and colleagues (2004), the validation study revealed also that the RAS total score and subscales are strongly correlated with the quality of life measure. Both the RAS total score (ranged from 41 to 205) and the five subscales’ scores were used as outcome measures in this study.
The Recovery Style Questionnaire (RSQ), the Italian version of Poloni et al. (2010), was used as a reliable and valid measure of McGlashan’s (1987) concept of recovery style, definable as the patients’ attitude to their mental illness, which is underpinned by the mechanisms of defence. It assesses «integration» and «sealing over» (McGlashan et al., 1975), which are two distinct coping styles placed along a continuum. An integrative recovery style is characterised by the patient’s awareness of the continuity in his mental activity and personality from before the symptomatologic experience, during the symptoms and through recovery. It was found to be associated with better social functioning (McGlashan, 1987). On the other hand, patients who «seal over» during recovery seem to isolate their symptomatologic experience. They view it as alien to their lives and are disinclined to allow any investigation of the symptoms. The questionnaire consists of 39 items, to which 13 subscales correspond, about attitudes to disorders: continuity, ownership, responsibility, curiosity, education, help-seeking, blame, cause, optimism, impact, fear, linking and satisfaction. For each item (for example, «I am curious about my illness»), people respond if they agree (yes) or disagree (no). An «integration» score (score = 1) is assigned on the subscale if the patient answers yes to either two or three items from the relevant subscale. In totalling the single subscale scores, it is possible to obtain an overall RSQ total score. The total number of «integrating» scores can be expressed also as a percentage of the total (e.g., 6 «integrating» subscales would be assigned a percentage score of 6/13 or 46 per cent). Moreover, a binary classification is possible: patients with scores between 0/13 and 6/13 were classified as «sealers»; those with scores between 7/13 and 13/13 as «integrators». Both the RSQ total score (ranged from 0 to 13) and the binary classification were used in this study.
Data analysis and results
Analytical plan
Firstly, in order to answer the first research question (evaluation of coherence), a specific checklist for the markers of recovery-oriented practices was created. Secondly, the transcripts of the in-depth interview with the MeNS coordinator and of the FGD with professionals were analysed by the «qualitative content analysis» (Hsieh & Shannon, 2005). Using each transcript as a unit for analysis, MeNS aims, peculiarities, methods and practices were compared with the recovery-oriented markers evidenced in the checklist in order to highlight how ROA goals and methods were contextualised in the MeNS programme.
As to the second research question (evaluation of effectiveness: patients’ perceived recovery), SPSS 24 was used to conduct all analysis. As a first step, preliminary descriptive statistics for demographics, clinical indicators and study variables were computed. Secondly, chi-square tests were carried out to identify whether significant differences existed between the compared groups, in terms of gender, age and clinical indicators. Thirdly, we compared the recovery scores in the different groups, at first using the two groups classification (A vs. B) and then replicated the analyses with the three groups classification (A, B1, B2), in order to control the effect of the context. In detail, we performed two separate ANOVA using the group as factor and both RSQ and RAS total scores as dependent variables. Finally, we computed both a Chi Square test using RSQ binary classification and a MANOVA using RAS subscales as dependent variables. In all the variance analyses, the scores of degrees of malfunctioning, motivation to change, compliance with treatment, therapeutic alliance and cooperation of family were used as covariates.
Regarding the third research question, (evaluation of effectiveness and social impact: quality of life and stigmatisation), both the transcript of the FGD with the MeNS beneficiaries and the documents selected to explore the social impact of the MeNS programme were used as a unit for analysis for the qualitative content analysis (QCA).
Evaluation of coherence: ROA markers in MeNS
The checklist described in Table 2 summarises the twelve markers of recovery-oriented practices. Some of them concern the role of staff and patients; others correspond to the goals of the rehabilitation path; many relate the features and management of the TRP.
Overall, QCA applied to the coordinator’s interview and the FGD with staff highlighted that all the markers of the recovery approach were identified in the evaluated programme. To better explain how they have been contextualised in the MeNS programme, we distinguish the coordinator’s and professionals’ representations emerging by QCA.
According to the coordinator, the ROA represents in the MeNS programme a «cultural attitude» because, differently from other models, MeNS staff use recovery-oriented methods and practices simultaneously with pharmacological treatments, also with people with very severe disorders. Professionals try to intervene globally, working on the person, on his/her context and on the illness, and also to share with each patient the nature of their disorder and the role of the drug used, in order to promote their awareness and avoid dependence on the experts. In this way, the user learns to know their disorder, is made aware of the global rehabilitation path and they are fully involved in all the process of care. Moreover, rehabilitation staff stimulate patients’ social inclusion promoting individual and group interventions within the psychiatric service, at the patient’s home or in other places of the community. Both the social network of the patients and cooperation among all the territorial stakeholders are promoted to encourage social inclusion processes, while psychoeducational interventions with families are provided to ensure shared purposes. The distinctiveness, in this model, is that the patient is the protagonist, and the staff present a guide to stimulate the highest level of patient’s autonomy; this last point constitutes both the aim of the TRP and an instrument used, from the start of the path, to improve patients’ quality of life. Focusing on people with SMI abilities, that is, on «what people with SMI can do rather than on their difficulties», staff encourage their self-determination and independence by guiding them in pleasant and personalised everyday social activities. Supported by the staff, they decide the activities in which they want to take part! So, by these methods and practices, they acquire instruments to be autonomous and self-determined.
According to health professionals’ representations, the ROA in the MeNS programme is evident from different features. Firstly, the goals are personalised on a case by case basis, within the general aim of improving patient autonomy, positive relationships and social inclusion; (b) the various social activities promoted to improve patients’ social inclusion and combat social stigma linked to mental illness, and the resulting opportunity for observing, monitoring and re-planning TRP; (c) the importance of a trust relationship between staff and patients, perceived as a precondition for establishing any goals and starting a positive change; (d) the focus on quality of life and social inclusion of people with SMI and on their potential, rather than on their disorder. For each of these aspects, specific significant quotes by professionals taken from the FGD transcript are listed below:
- «… the goals could not be standardised; they are set according to the potential of each person» (psychiatric rehabilitation therapist).
- «Through group activities, those with SMI start to relate to others, express themselves and learn social dynamics! The MeNS programme works in society, in the context of the patients, with their families… we act as a kind of “day-centre in society”» (psychologist); «… in this way there isn’t a gap between the rehabilitation treatment and the “real word”» (health educator); «… we can observe people with SMI in the real word, so we can have feedback and work on their potentials and limits; according to these, we readapt the goals of the intervention and co-construct with the patient a plan for achieving them» (psychiatric rehabilitation therapist).
- «The staff become a helper group for the patient, the professionals are like caregivers … before establishing any goal, the staff work with a view to building a relationship of trust with the patient; this “therapeutic alliance” is a basic prerequisite of any form of rehabilitation path … If people with SMI don’t trust us, no work is possible! In this way, little by little, they reactively trust in others, in the service, in themselves … after a period of social loneliness, they’re gradually more likely to ask for help, and this represents an initial and essential change!» (psychologist).
- «In recovery-oriented practices, we encourage people with SMI to live a “normal life in their context,” regardless of their mental illness; so, the focus is on their everyday life, house, job and free time. We are interested in people with SMI being present in society, and consequently in their integration into society» (psychiatrist); «… If patients become able to listen, participate, work, use the bus, manage their house, they can have a purpose in their life, a good quality of life beyond their symptoms, even if a significant reduction of their symptoms was not recorded» (psychologist); «… for MeNS beneficiaries, the advantage is that we focus on each person rather than on the mental disorder; we work on their abilities and potential rather than on their problems: what can you do very well? Ok, let’s start from this!» (health educator).
Evaluation of effectiveness in terms of recovery
Table 3 summarises the descriptive statistics for the demographic variables and clinical indicators, both for the total sample and for the two-groups and three-groups classification. Table 4 describes the descriptive statistic for the study observed variables.
Preliminary analyses highlighted no significant differences between the two examined groups (A vs. B) with regard to gender (χ(1)=.15; p=n.s.) and age (F(1, 149)=.5; p=n.s.). No statistically significant differences for gender (χ(2)=3.28; p=n.s. ) and age (F(2, 149)=.56; p=n.s.) distribution were observed also when the three groups were compared (A vs. B1vs. B2). As regards the five clinical indicators assessed by clinicians, significant differences emerged only in terms of degree of malfunctioning (χ(4)=19.17; p=.001) and compliance with treatment (χ(4)=13.39; p=.01), when the three groups comparison was made. Therefore, we used all the clinical indicators as covariate variable in the sequential analysis.
ANOVA using the group as factor evidenced no difference between the two groups (A vs. B) in RSQ total score (p≥ .05). Also the difference in the binary classification is non- significant (χ(1)=.13; p=n.s.); however, most of the participants (66%) are classified as integrators. On the other hand, a significant difference in RAS total score (F(1, 148)=25,07; p≤ .001, η2= .16) was found, with higher levels of recovery in group A (EMMs = 160.30) compared to group B (EMMs Gc= 132.95). MANOVA using both the RAS total score and the RAS subscales scores as dependent variables resulted in a significant multivariate effect of the group [Wilks’ Lambda = .80, F(1, 148) = 5.35, p ≤.001, partial η2= .20]. Univariate analysis showed that the treatment group had a significant effect on RAS total score [F(1, 148) = 23.93, p ≤ .001, partial η2= .15], «willingness to ask for help» subscale [F(1, 148)=4.31; p≤ .05, partial η2=.03] (Figure 1) and «reliance on others» subscale [F(1, 148)=4.55; p≤ .05, partial η2= .033] (Figure 2), but not for the other RAS subscales.
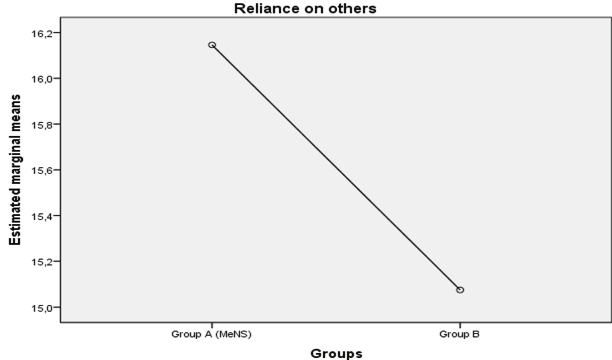
Fig. 1 The effect of the treatment group on «willingness to ask for help» subscale (the covariate variables in the model will be evaluated according to the following values: cooperation of family = 1,79; degree of malfunctioning = 2,21; motivation to change = 2,17; compliance with treatment = 2,45; therapeutic alliance = 2,45).
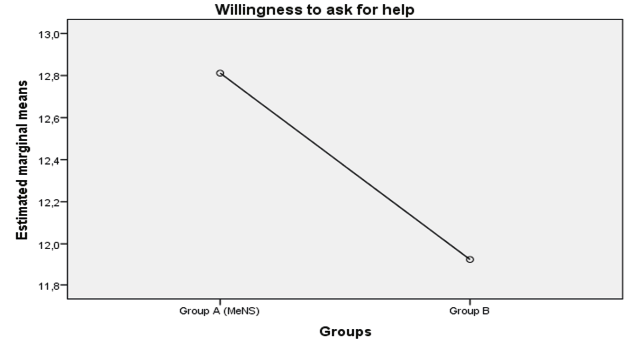
Fig. 2 The effect of the treatment group on «reliance on others» subscale (the covariate variables in the model will be evaluated according to the following values: cooperation of family = 1,79; degree of malfunctioning = 2,21; motivation to change = 2,17; compliance with treatment = 2,45; therapeutic alliance = 2,45).
Comparing the three groups (A vs. B1 vs. B2), results of ANOVA evidenced no differences in RSQ total score (p≥ .05). However, a significant difference in RAS total score (F(2, 148)=30.03; p≤ .001, η2= .37) was found, with higher levels of recovery in the group A (EMMs = 160.07) compared both to the group B1 (EMMs = 152.38) and to the Group B2 (EMMs = 113.38).
MANOVA using both the RAS total score and the RAS subscales scores as dependent variables resulted in a significant multivariate effect of the group [Wilks’ Lambda = .47, F(2, 148) = 9.72, p ≤.001, partial η2= .31]. Using the three groups classification, univariate analysis showed that the treatment group had a significant effect on RAS total score [F(2, 148) = 38.36, p ≤ .001, partial η2= .37], but not for the singles RAS subscales.
Evaluation of the effectiveness and social impact in terms of quality of life and social stigmatisation
Results evidenced by QCA applied to the patients’ FGD highlighted a moderately perceived effect of the MeNS programme on their quality of life and social stigmatisation. Narrating their life stories, some of those interviewed with SMI thought «this couldn’t get any worse» Before the MeNS experience, they described themselves as discouraged and helpless: some said they had no contact with social contexts, they did not work and did not have any interpersonal relationships. Thanks to the MeNS staff, they described feeling «encouraged, supported and guided step by step, first to do small things — for example, walk out of the home, buy something, meet somebody — and later, to resume a normal life». For all the interviewees, having a positive and intense relationship with staff has been very important. «When I got here — says a patient — first of all I got started, I started to meet people, do activities … but at the beginning, I couldn’t move myself and they (the staff) drove me to and from my home … gradually, I felt more confident … and I started to live again!».
Starting to live again has a specific meaning in the life stories of each person with SMI involved in recovery-oriented TRP. Describing their significant practices and activities, one of the interviewed, for example, declares that, after much effort, he was able to study again and get a degree; another MeNS user describes her satisfaction with the opportunity to get to work after a long period of loneliness; another states that he was hired for the first time at a health products shop, thanks to an internship organised within the MeNS programme. In all the stories, MeNS beneficiaries believe that they have achieved significant improvements to their quality of life; thanks to their achievements, they felt they were autonomous and successful people. Moreover, thanks to the opportunity to work, FGD participants felt less stigmatised by society, because they were able to live an independent and dignified life despite their mental disorder.
This perceived effect is reflected also throughout the analysed documents; they explain more effectively what the MeNS programme was trying to do: helping users and the community to realise that people with SMI are persons having citizenship and job rights, people able to be productive persons if adequately supported. In this vein, the social stigma related to mental disorder was undermined so that MeNS users were not marginalised and stigmatised because of their mental disorder, but socially integrated citizens. In order to achieve this final aim, the MeNS programme guaranteed all users the opportunity to participate in different socio-recreational and labour activities: some local journals describe, for example, users’ visits to churches and local places of cultural interest organised «to take them out of the physical space of MHS and place them in a new mental space».
Thus, the integration process and the fight against social exclusion and discrimination based on social stigma becomes a cultural challenge. The innovative approach, as we read in local newspapers, «combines the “care” (medical dimension) with prevention and rehabilitation, made possible by the promotion of cultural events and activities such as theatre, cinema, sport events, exhibitions…» This has meant a radical change in the way of working, as different public and private stakeholders started collaborating in a new way to reduce social stigma and the self-stigma of persons with SMI. Through this integrated method, which invests in the quality of life of those with SMI, thanks to the opportunities provided within their region, the workload of their caregivers is reduced; therefore, also families’ stress decreases, as users become increasingly independent. As user autonomy is the main focus of the MeNS programme, thanks to an agreement with the local Jobcentre, MeNS users have been involved in one-year traineeships in cooperation with a local hospice, where they learn social competences through front-office activities. In the same way, a desk for socio-labour inclusion open to all the citizens, rather than only vulnerable social groups, was set up in the MSH where the MeNS programme was initiated.
Taken as a whole, the socio-recreational activities organised by MeNS staff in cooperation with local cultural operators, and the work experience guaranteed to MeNS participants seem to have produced a positive effect both on self-perceived stigma and quality of life, and on the social stigma associated with mental illness.
Discussion
The aim of this study was to investigate the coherence, effectiveness and social impact of a recovery-oriented programme who, within a relational social work perspective, aims at combatting patients’ stigmatisation and social exclusion and promoting their recovery and quality of life. Thus, the results of this evaluative research will be discussed both within the framework of ROA and considering the principles of RSWP.
Regarding the first research question (evaluation of coherence), qualitative data showed that MeNS programme is consistent with a ROA, as MeNS vision, goals, methods, and practices present the markers of a recovery-oriented model (Table 2). MENS mental health practitioners, indeed, support users’ capabilities and their trust, stimulate the involvement of their families, and act as facilitators for their interactions with the outside world. According to a strength approach rather than a deficit model, interventions focused on patients’ coping and abilities rather than on their disorder, were realized also with users with at-risk mental states. These core-aspects of the MeNS programme recall some key-principles of the relational perspective, according to which helping process is a co-construction path in which professionals act as helpers (Raineri & Cabiati, 2016), that is help users interact with community and, in their role of «relational guide», facilitate their decisions, accompanies their actions, and support them in problems’ coping (Folgheraiter, 2015). In line with the RPSW, the helping relationship in MeNS programme is based on the reciprocity principle, as practitioners cede some power to the less empowered people with SMI, so that they become more autonomous and active in dealing with their problems (Folgheraiter & Raineri, 2017). Furthermore, consistent with a ROA (e.g. Vita et al., 2016), MeNS interdisciplinary team designs interventions which are as integrated as possible within users’ everyday life context, both to help the network to develop its welfare role (Folgheraiter & Raineri, 2012), and to improve users’ autonomy, quality of life, self-determination and social inclusion. These latter key-elements of the recovery-oriented programme recall the concept of relational empowerment expressed in RPSW and appear coherent with its central idea that the «change emerges from a reciprocal aid, both between people in difficult circumstances, family members, friends and neighbours, and between the network and the social worker» (Raineri & Cabiati, 2016, p.1005).
As regards the second research question (evaluation of effectiveness in terms of patients’ perceived recovery), our findings highlighted that MeNS users show higher levels of RAS total score compared to patients involved in traditional pathways to care and rehabilitation, both when other MHSs were considered (B2 group) and when the same MHS where the MeNS programme was experienced was considered (B1 group). This means that thanks to recovery-oriented methods and relational practices, users experienced new skills and positive social roles, developed personal comfort (Ralph, 2000) and a new purpose in life (Davidson, 2012), thereby being able to live a satisfying, hopeful and meaningful life as citizens of their communities, beyond the limitations due to their psychiatric symptoms (Anthony, 1993; Deegan, 1993). Likewise, the significant differences between the A and B groups, also in the «willingness to ask for help» and «reliance on others» subscales, indirectly confirm the central role of trust bonding of MeNS beneficiaries with mental health practitioners as mechanism to promote recovery as a process. Through the lens of the RSWP, these findings suggest that in MeNS programme the relationship was used as a change agent (Tosone & Gelman, 2017), as beneficiaries’ experiences of hope and empowerment emerge at the relation with the environment, and especially within the helping process. This conceptualization, consistent with the literature which emphasized the decisive role of the social relationships for the wellbeing of people with SMI (Schön et al., 2009), highlights the irreducibly relational nature of recovery (Price-Robertson, Obradovic, & Morgan, 2017) and underlines that users’ positive changes in self-perception and identity are interpersonal processes.
However, data show that recovery gap between patients involving in MeNS group (A group) and those involved in traditional rehabilitation models treated in the same MHS (B1 group) was smaller than the recovery gap between MeNS patients and those treated by traditional TRP in other MHSs (B2 group). Regarding this result, it is possible to suggest that MeNS professionals are more capable of working with a view of empowerment and positive change, even when they implement traditional TRP, probably because their «sensibility» and «cultural attitude» in using recovery-oriented approach and relational paradigm tacitly influence their practices in the service, that is their way of being and working with users. If we used the recovery concept in the sense of a guideline to transform the mental health system (Anthony, 1993), the key role that the organisational culture of MHSs has in stimulating ROA (Ardvisson & Ardvisson, 2005) is evident. Similarly, we suggest that professionals who share the principles of RSWP can use their relationship with users as basis for change, also when people with SMI were involved in traditional rehabilitation paths. Thus, the role of the context in which the PTR was made is an important variable, as well as the type of treatment received. In this line, it is important to underline that although MeNS patients show no greater integration compared to the comparison groups, most participants of this sample are classified as integrators. Therefore, in line with studies which found no significant statistical difference in RSQ between patients receiving different types of treatment (e.g., Fitzgerald, 2010), we can hypothesize that all the rehabilitation activities promoted within the context of MHSs may be enough to encourage the integration coping strategy (McGlashan, 1987). However, target studies could shed light on other factors influencing these results, including methodological aspects.
Finally, as regards the third research question (evaluation of quality of life and social impact), MeNS patients who took part in the FGD described a lower stigmatisation and better quality of life, thanks to the programme. These results are consistent with data from the analysed journal articles and highlighted the programme’s capacity to combat social stigmatisation and consequent social exclusion. In particular, MeNS programme seems to encourage active inclusion of people with SMI in society and avoiding their stigmatisation, both by cultural and social activities in the community and by improving their employment opportunities. Both these elements, which are key aspects of the rehabilitation process, are made possible by the «relational guide» of mental health practitioners, who support people with SMI in their social interactions, as well as in having meaningful goals in their life. Although this is not a longitudinal study, in keeping with literature highlighting the association between poor recovery, self-stigma and greater symptoms (Espinosa et al., 2016; Tait et al., 2003), we can suggest that, thanks to MeNS activities and helping process based on a reliance relationship, patients gradually become more likely to participate actively in the life of their community, reducing their self-stigma. Initially with the professional support and the facilitator role of practitioners, and then autonomously, they experience new forms of social interaction, face up to social and self-stigmatisation barriers (Ritsher et al., 2003), and thereby promote their own abilities. Thus, the cycle of discrimination due to mental health problems is broken, the patients’ quality of life is improved (Tansella & Thornicroft, 2009), and the community attitude and behaviour towards them change for the positive (Couture & Penn, 2003).
Overall, the current study highlighted that MeNS programme, in keeping with the European recommendations (European Commission, 2010), is able to reduce social stigma of people with SMI and improve their social inclusion, by combining recovery-oriented activities with initiatives based on a community-based approach, within a relational framework. The principles of the RSWP, such as reciprocity, empowerment, recognition of experiential knowledge, and participation of service users in the planning of their care interventions (Raineri, 2017), indeed, seem to guide implicitly recovery-oriented practices within MeNS programme, which promote coping networks actions to increase users’ well-being.
Although this study is preliminary and not without weaknesses, our results can have important implications for policy and organisation of services: they emphasised the importance of disseminating recovery-oriented methods and practices in Italian MHSs and underline the role of the context in which each type of rehabilitation path is implemented, thus encouraging mental health directors and policymakers to reflect on how to design effective recovery-oriented programmes and services. To promote effective recovery oriented treatments (Jacobson & Greenley, 2001), rehabilitation services should aim at promoting among patients those life skills necessary for integration within the community to which they belong (Rössler, 2006) and help them recover a role in their family, social groups and society (Liberman, 2008). Moreover, for recovery to be fully integrated into clinical practice, an environment that embraces recovery values (e.g. self-determination, social inclusion, personalised care plan) in all organisational processes is crucial (Farkas, 2007).
If, on the one hand, recovery represents a holistic approach to wellness («a cultural attitude»), on the other hand, it is increasingly important that mental health specialists have a clear understanding of recovery principles (Jääskeläinen et al., 2012) and relational methods (Folgheraiter, Calcaterra, & Cabiati, 2020). Therefore, adequate training should be guaranteed for all professionals working in MHSs aiming to implement a recovery-oriented organisation model, so that they are able to focus on user strengths and social networks to promote positive change beyond their mental disorder. Finally, regular monitoring and evaluation studies should be planned to examine the MHS’s capacity to promote users’ recovery and wellbeing. Stronger cooperation between mental health professionals, researchers and policymakers could help improve the quality of the MHS, and thereby the quality of life of their users.
References
Allott, P., Loganathan, L., & Fulford, K. W. M. (2009). Discovering hope for recovery. Canadian Journal of Community Mental Health, 21(2), 13-33.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders: DSM-5, 5th ed. Washington DC: American Psychiatric Association.
Anthony, W.A. (1993). Recovery from mental illness: The guiding vision of the mental health service system in the 1990s. Psychosocial Rehabilitation Journal 16(4), 11-23.
Arvidsson, H., & Arvidsson, E. (2005). Recovery from severe mental illness: a 5-year follow-up study after the 1995 Swedish mental health care reform. Scandinavian Journal of Disability Research 7(2), 91-108.
Boggian, I., Lamonaca, D., Ghisi, M., Bottesi, G., Svettini, A., Basso, L., Bernardelli, K., Merlin, S., Liberman, R.P., & S.I.R. 2 group (2020). The Italian Study on Recovery 2 Phase 1: Psychometric Properties of the Recovery Assessment Scale (RAS), Italian Validation of the Recovery Assessment Scale. Frontiers in psychiatry. doi:10.3389/fpsyt.2019.01000.
Boggian, I., Lamonaca. D., Svettini, A., Ghisi, M., & Gruppo SIR (2011). Studio Italiano sul Recovery — SIR. Fase 1: applicazione italiana della Recovery Assessment Scale. Psichiatria di Comunità, X(1), 38-48.
Bonney, S. and Stickley, T. (2008). Recovery and mental health: a review of the British literature. Journal of psychiatric and mental health nursing, 15(2), 140-153.
Cavelti, M., Kvrgic, S., Beck, E.M., Kossowsky, J., & Vauth, R. (2012). Assessing recovery from schizophrenia as an individual process. A review of self-report instruments. European psychiatry, 27(1), 19-32.
Clementi, S. (2019). Working Together Responsibly: An evaluation research of FARE’s program on mental illness. Relational Social Work, 3(2), 60-71
Corrigan, P.W, Giffort, D., Rashid, F., Leary, M., & Okeke, I. (1999). Recovery as a Psychological Construct. Community Mental Health Journal 35(3), 231-239.
Corrigan, P.W., & Ralph, R.O. (2005). Introduction: Recovery as Consumer Vision and Research Paradigm. In R.O. Ralph, & P.W. Corrigan (Eds.), Recovery in mental illness: Broadening our understanding of wellness (pp. 3-17). American Psychological Association.
Couture, S.M., & Penn D. (2003) Interpersonal contact and the stigma of mental illness: A review of the literature. Journal of Mental Health, 12(3), 291-305.
Davidson, L. (2012). Considering recovery as a process: or life is not an outcome. In A. Rudnick (Ed.), International perspectives in philosophy and psychiatry. Recovery of people with mental illness: Philosophical and related perspectives (pp. 252-263). Oxford: Oxford University Press.
Deegan, P.E. (1993). Recovering our sense of value after being labelled mentally ill. Journal of psychosocial nursing and mental health services, 31(4), 7-11.
Drapalski, A.L., Lucksted, A., Perrin, P.B., Aakre, J.M., Brown, C.H., DeForge, B.R., & Boyd, J.E. (2013). A model of internalized stigma and its effects on people with mental illness. Psychiatric services, 64(3), 264-269.
Espinosa, R., Valiente, C., Rigabert, A., & Song, H. (2016). Recovery style and stigma in psychosis: the healing power of integrating. Cognitive Neuropsychiatry, 21(2), 146-155.
European Commission (2010). Promoting Social Inclusion and Combating Stigma for better Mental Health and Well-being. Background document to the European Commission thematic conference. Available on line: https://ec.europa.eu/health/sites/health/files/mental_health/docs/ev_20101108_bgdocs_en.pdf.
Farkas, M. (2007). The vision of recovery today: what it is and what it means for services. World psychiatry: official journal of the World Psychiatric Association (WPA), 6(2), 68-74.
Fitzgerald, M.M. (2010). Comparison of recovery style and insight of patients with severe mental illness in secure services with those in community services. Journal of Psychiatric and Mental Health Nursing, 17(3), 229-235.
Folgheraiter, F. (2011). Fondamenti di metodologia relazionale: La logica sociale dell’aiuto. Trento: Erickson.
Folgheraiter, F. (2015). Relational social work. In J. D. Wright (Ed.), International Encyclopedia of the Social & Behavioral Sciences (Vol. 20, pp. 221-226). Oxford: Elsevier.
Folgheraiter, F., & Raineri, M. L. (2012). A critical analysis of the social work definition according to the relational paradigm. International Social Work, 55(4), 473-487.
Folgheraiter, F., & Raineri, M.L. (2017). The principles and key ideas of Relational Social Work. Relational Social Work, 1(1),12-18.
Folgheraiter, F., Calcaterra, V., & Cabiati, E. (2020). Adults, families and social networks in the relational social work method. In J. Parker, & S. Ashencaen Crabtree (Eds.), Human Growth and Development in Adults: Theoretical and Practice Perspectives (pp. 63-80), Policy Press.
Hsieh, H.F., & Shannon, S.E. (2005). Three Approaches to Qualitative Content Analysis. Qualitative Health Research, 15(9), 1277-1288.
Jääskeläinen, E., Juola, P., Hirvonen, N., McGrath, J.J., Saha, S., Isohanni, M., Veijola, J., & Miettunen, J. (2013). A systematic review and meta-analysis of recovery in schizophrenia. Schizophrenia bulletin, 39(6), 1296-1306.
Jacobson, N., & Greenley, D, (2001). What is recovery? A conceptual model and explication. Psychiatric services, 52(4), 482-485.
Kern, R.S., Glynn, S.M., Horan, W.P., & Marder, S.R. (2009). Psychosocial treatments to promote functional recovery in schizophrenia. Schizophrenia bulletin, 35(2), 347-361.
Layard, R. (2006). The case for psychological treatment centres. British Medical Journal, 332, 1030-1032.
Leete, E. (1989). How I perceive and manage my illness. Schizophrenia Bulletin, 15(2), 197-200.
Liberman, R.P. (2008). Recovery from disability: Manual of psychiatric rehabilitation. Washington, DC: American Psychiatric Publishing, Inc.
McGlashan, T.H. (1987). Recovery style from mental illness and long-term outcome. Journal of Nervous and Mental Disease, 175(11), 681-685.
McGlashan, T.H., Levy, S.T., & Carpenter, W.T. (1975). Integration and sealing over: Clinically distinct recovery styles from schizophrenia. Archives of General Psychiatry, 32(10), 1269-1272.
McLoughlin, K.A., & Fitzpatrick, J.J. (2008). Self-reports of recovery-oriented practices of mental health nurses in state mental health institutes: Development of a measure. Issues in Mental Health Nursing, 29(10), 1051-1065.
O’Connell, M., Tondora, J., Croog, G., Evans, A., & Davidson, L. (2005). From rhetoric to routine: assessing perceptions of recovery-oriented practices in a state mental health and addiction system. Psychiatric rehabilitation journal, 28(4), 378-386.
Poloni, N., Callegari. C., Buzzi. A., Aletti, F., Baranzini, F., Vecchi, F., & Vender, S. (2010). The Italian version of ISOS and RSQ, two suitable scales for investigating recovery style from psychosis. Epidemiology and Psychiatric Sciences, 19(4), 352-359.
Price-Robertson, R., Obradovic, A., & Morgan, B. (2017). Relational recovery: beyond individualism in the recovery approach. Advances in Mental Health, 15(2), 108-120.
Raineri, M. L. (2017). Relational Social Work and mutual/self-help groups. Relational Social Work, 1(1), 19-38.
Raineri, M. L., & Cabiati, E. (2016). Kitwood’s thought and relational social work. European Journal of Social Work, 19(6), 1004-1020.
Ralph, R.O. (2000). Recovery. Psychiatric rehabilitation skills, 4(3), 480-517.
Ritsher, J.B., Otilingam, P.G., & Grajales, M. (2003). Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry research, 121(1), 31-49.
Roberts, G., & Hollins, S. (2007). Recovery: our common purpose? Advances in Psychiatric Treatment, 13(6), 397-399.
Roe, D., Rudnick, A., & Gill, K.J. (2007). The concept of “being in recovery”. Psychiatric Rehabilitation Journal, 30(3), 171-173.
Roessler, W. (2006). Psychiatric rehabilitation today: an overview. World Psychiatry, 5(3), 151-157.
Rudnick, A. (Ed.) (2012). Recovery of people with mental illness: Philosophical and related perspectives. Oxford: Oxford University Press.
Salyers, M.P., & Tsemberis, S. (2007). ACT and recovery: Integrating evidence-based practice and recovery orientation on assertive community treatment teams. Community Mental Health Journal, 43(6), 619-641.
Shamir, E. (2012). Families and patients with mental illness: on the recovery road. In A. Rudnick (Ed.), Recovery of people with mental illness. Philosophical and related perspectives (pp. 39-57). Oxford: Oxford University Press.
Shepherd, G., Boardman, J., & Burns, M. (2010). Implementing recovery. A methodology for organisation change. London: Sainsbury Centre for Mental Health.
Tait, L., Birchwood, M.A.X., & Trower, P. (2003). Predicting engagement with services for psychosis: insight, symptoms and recovery style. The British Journal of Psychiatry, 182(2), 123-128.
Tansella, M., & Thornicroft, G. (2009). Implementation science: understanding the translation of evidence into practice. The British Journal of Psychiatry, 195(4), 283-285.
Tosone, C. & Gelman, C. R. (2017). Relational Social Work: A Contemporary Psychosocial Perspective on Practice. In F. J. Turner, (Ed.) Social work treatment: Interlocking theoretical approaches (pp. 420-427), Oxford University Press.
Unzicker, R. (1989). On my own: A personal journey through madness and re-emergence. Psychosocial Rehabilitation Journal, 13(1), 71-77.
Vita, A., & Barlati, S. (2019). The implementation of evidence-based psychiatric rehabilitation: challenges and opportunities for mental health services. Frontiers in Psychiatry, 10, 147.
Vita, A., Corrivetti, G., Mannu, J., Semisa, D., & Viganò, C. (2016). Psychosocial rehabilitation in Italy today. International Journal of Mental Health, 45(1), 15-23.
Xu, Z., Lay, B., Oexle, N., Drack, T., Bleiker, M., Lengler, S., Müller, C., Mayer Brooke, M., Rössler, W., & Rüsch, N. (2019). Involuntary psychiatric hospitalisation, stigma stress and recovery: a 2-year study. Epidemiology and psychiatric sciences, 28(4), 458-465.
Author and article information
Balenzano, C., & Moro, G. (2021). Mental illness and social exclusion: An evaluation of a recovery-oriented rehabilitation programme. Relational Social Work, 5(1), 11-33, doi: 10.14605/RSW512102.

Relational Social Work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License


